


On the basketball court, Audrey Biggs is known for her versatility, tenacity, and incredible teamwork. The same spirit that propelled her to success as a top-scoring starting forward is exactly what has helped her navigate one of the toughest challenges of her life.
“I was playing for the West Virginia Thunder traveling team. I went up for a layup with another player on my back,” Audrey said. “I came down hard and felt a pop. I let out a scream, which is something I never do — I’m not the crying type. But I knew something was wrong.”
Audrey tore her anterior cruciate ligament (ACL) and was terrified of what that might mean for her future as an athlete and her goal to play college basketball.
“My mental state was not okay. My dad had a serious conversation with me. He said that ‘things happen for a reason. You will get through this and come back as a better version of yourself,’” Audrey said. “So, I decided to improve my mindset and focus on my goals. I wanted to play at the highest level I possibly could, and I was not going to let this injury stop me.”

Audrey turned to surgeon and Assistant Professor of Orthopedics at Marshall University, Chad D. Lavender, MD (Huntington, WV), for help.
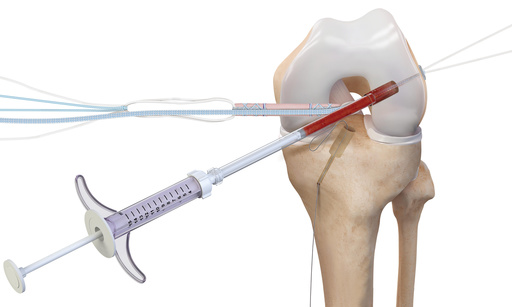
“Audrey’s injury was straightforward, but we were up against the clock to get her back on her feet and ready for the college recruiting process,” Dr. Lavender said. “We performed a QuadLink™ BioACL™ reconstruction using a quad tendon for her new ACL (graft) and FiberTag TightRope implants. We then augmented the reconstruction using the InternalBrace™ technique.”
The BioACL reconstruction technique involves harvesting bone marrow from the patient’s shin bone, which is then spun into bone marrow aspirate. The bone marrow aspirate is added to a mixture of autograft and allograft bone to form a putty that the surgeon puts into the knee socket before pulling in the ACL graft.
“Essentially, we are fertilizing the socket with good cells and bone grafting. I liken it to a potted-plant-like technique,” Dr. Lavender said. “In a study my team conducted, the biologics help improve the healing process and the InternalBrace technique allows for a faster return to rehab. We have shown very high patient-reported outcomes as well as return to sport after the BioACL technique”.¹
With her fitness and commitment to return to playing competitive basketball, Audrey jumped in. She went to therapy five days a week with fierce determination.


“I decided, I’ve got this. I am striving to be one percent better every single day,” she said. “Dr. Lavender was like a coach to me. He was there for me every step of the way and I told him, ‘I’ve got this—I am coming back stronger and better.’”
Just six months after her injury, Audrey was not only back on the court, but she was playing so well, she signed on to play Division I basketball at the University of Pittsburgh.
“Audrey is remarkable,” Dr. Lavender said. “She performed so well, so fast, she got back and earned new Power Five conference offers. When you can help someone get back to what they love, that is so special.”
Today, Audrey says she is living proof that there is hope after an ACL injury, which is far too common in sports like basketball.
“If you have a goal, if you have a dream, don’t let an injury like this stop you,” she said. “Get the right medical team on your side and it can just be a bump in the road.”
Reference
1. Lavender C, Hewett T, Johnson J, Peluso R, Patel T, Taylor S. Return to activity following ACL reconstruction with the fertilized ACL: a retrospective study. Marshall J Med. 2023; 9(3). doi:10.33470/2379-9536.1410